FAQ about tailbone pain
The most aksed questions about tailbone pain – causes, advise and treatment and phsyiotherapy for tailbone pain
This page gives you the answers tot he most asked questions about tailbone pain. The information is meant for people with coccyx pain that want to understand where their problems come from, what they can do themselves and what treatment options there are for tailbone pain.
The explanations are based on my experience as specialised therapist of tailbone pain. Where relevant I will refer to pages with more elaborate information here at tailbonetherapist.com.
On this page you will find the answer to the following questions:
- What is tailbone pain?
- Is there inflammation in my tailbone?
- What causes tailbone pain?
- Where does the pain in tailbone pain come from?
- Why is sitting so painful with tailbone pain?
- What is the difference between a bruised and a fractured tailbone?
- Can stress cause tailbone pain?
- Can tailbone pain be something serious?
- When should I be concerned about tailbone pain?
- Why does tailbone pain often last so long?
- What should I avoid doing with tailbone pain?
- What is helpful to do with tailbone pain?
- What is the best way to sit with tailbone pain?
- Can I cycle or ride a scooter with tailbone pain?
- Can I exercise with tailbone pain?
- Should I see my GP for tailbone pain?
- Should I take pain medication for tailbone pain?
- Can tailbone pain resolve on its own?
- Does tailbone pain always need treatment?
- Can anything be done about tailbone pain?
- What treatments are available for tailbone pain?
- Why are so few professionals specialised in tailbone pain?
- Does physiotherapy help with tailbone pain?
- What does physiotherapy for tailbone pain look like?
- What does medical treatment by a doctor involve?
- Are tailbone treatments painful?
- What if imaging shows no abnormalities in the tailbone?
- An abnormality is seen on the scan – what does that mean?
- What can be done if the tailbone is misaligned?
- What can be done about tailbone deformities?
- Can anything be done if the tailbone is fractured?
- Can tailbone pain be treated during pregnancy?
- What if previous treatments have not helped?
- How long does it take for tailbone pain to resolve?
- What can I do myself to reduce tailbone pain?
- Should I buy a tailbone cushion?
- Which exercises help with tailbone pain?
- Do I have a weak spot once I’ve had tailbone pain?
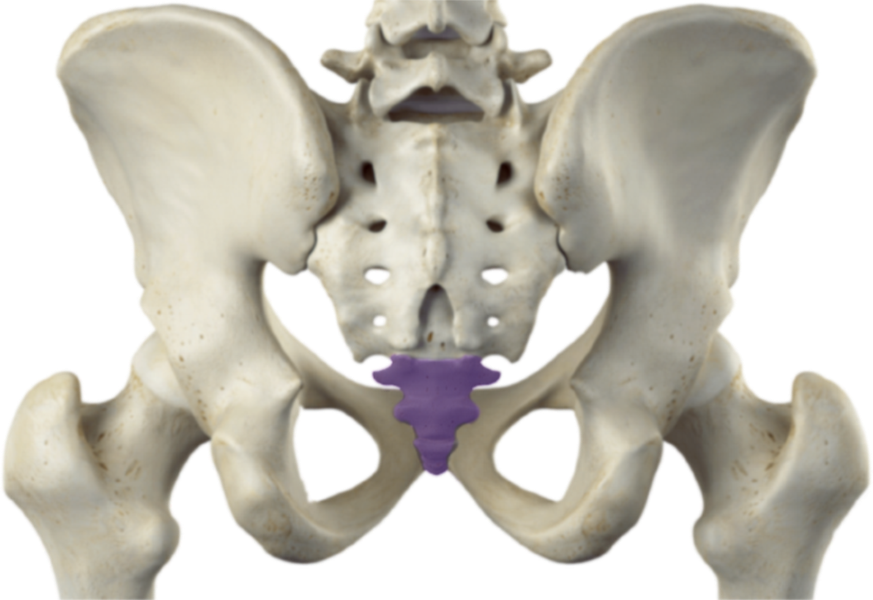
1. What is tailbone pain?
Tailbone pain is pain around the coccyx, usually just behind the anus, which often increases when sitting or when pressure is applied to the tailbone.

The pain may remain local but can also radiate to surrounding areas.
Tailbone complaints are typically characterised by pain when sitting, standing up, or when direct pressure is applied to the tailbone. Symptoms can range from mild discomfort to severe limitations in daily functioning. On the in-depth page about tailbone pain, the development and course of these complaints are explained in more detail.
2. Is there inflammation in my tailbone?
Yes, with tailbone pain there is almost always an inflammatory response, but this is usually a consequence rather than the cause of the problem.
Any form of overload in the body is accompanied by inflammation, and this also applies to the tailbone. This inflammatory response is part of the body’s natural healing mechanism. Suppressing inflammation may temporarily reduce pain, but often does not resolve the underlying issue and may even delay recovery. Effective treatment for tailbone pain therefore requires looking beyond inflammation alone. More about that will be explained in the page about Treatment.
3. What causes tailbone pain?
The cause of tailbone pain is often mechanical overload of the tailbone, although a clear cause cannot always be identified.
Overload may occur after a direct impact, such as a fall onto the tailbone, or due to internal stress, for example during or after childbirth. Prolonged or poor sitting posture, as well as changes such as pregnancy, can also contribute.
In many cases, however, no obvious cause is found. The underlying issue is then usually reduced or impaired movement of the tailbone. This reduced mobility can cause pain even without visible damage and is a key focus of physiotherapy for tailbone pain. More about that you can find on this page.
4. Where does the pain in tailbone pain come from?
Pain in tailbone pain usually results from overload of the structures of and around the tailbone rather than from serious abnormalities.
In most cases, the problem lies in how the tailbone functions and moves, not in fractures, tumours, infections or structural abnormalities. Even when imaging appears abnormal, these findings are often not the direct cause of pain.
Therefore, treatment usually focuses on improving mechanical function rather than structural changes. Because physicians mostly focus on structural problems and diseases, the expertise of physiotherapists and other manually working therapists is with the movement and function of the tailbone. Specialists in this area are rare and here at tailbonetherapist.com you can easily find a specialist at the page Appointment.
5. Why is sitting so painful with tailbone pain?
Sitting is painful because it places direct pressure on the tailbone, especially when it is overloaded or irritated.
Sitting compresses the tailbone and this can cause or aggreviate pain. As soon as the sitting position is left, the pain mostly quickly reduces, although the rising from sitting itself can be sensitive. The exact biomechanics is explained in detail in the video’s about tailbonepain and these you can find in this page.
6. What is the difference between a bruised and a fractured tailbone?
With a bruised tailbone the bone is intact; with a fracture it is not, but recovery is often similar.

A bruise usually results from impact or spraining of the small joints of the tailbone, comparable to a sprained ankle. As well as with a fracture, recovery typically occurs naturally, provided the conditions for healing are present.
Imaging such as X-rays rarely has extra value because it doesn’t change the treatment trajectory. Practical tips to relief the tailbone in the acute phase and after, you can find at the page with Tips.
7. Can stress cause tailbone pain?
Yes, stress can be an important cause or contributing factor in tailbone pain.
Stress affects the entire body, but the tailbone region is particularly sensitive. The pelvic floor muscles are often among the first to tense under stress, and this increasing tension leads to an increased pull directly on the tailbone and can disrupt its function, which can provoke or maintain pain.
Here at tailbonetherapist.com you can find exercises that are aimed at relaxation of the pelvic floor and in general to break the stress cycle. They can be found at this page.
8. Can tailbone pain be something serious?
In rare cases, tailbone pain may have a serious underlying cause, but this is uncommon.
Examples include tumours or bone infections. These conditions are usually accompanied by additional warning signs such as unexplained weight loss, night pain or a history of infection. The pain is often not influenced by posture or pressure. Medical evaluation is essential in such cases.
Where we therapist can think along in exclusing these severe causes, the expert here is your doctor.
9. When should I be concerned about tailbone pain?
Concern is mainly warranted when tailbone pain is accompanied by warning signs and does not change with posture or pressure.
Think of pain that doesn’t change with sitting, standing or lying down or symptoms that need medical examination such as fever, night pain or unexplained weight loss.
If the pain is purely local and does not resolve despite favourable conditions, there is usually no cause for concern, but assessment by a specialised therapist is advisable. You can find one through the page Appointment.
10. Why does tailbone pain often last so long?
Tailbone pain often persists because appropriate treatment is lacking.
Many people are told nothing can be done about coccyx pain or receive only symptom-based treatment. Specialised knowledge of tailbone pain is limited, meaning targeted therapy is often applied delayed or not at all, even though appropriate functional treatment can be highly effective.
If you are looking for a specialised therapist, you can find one at the page Appointment.
11. What should I avoid doing when I have tailbone pain?
Avoid anything that triggers or worsens the tailbone pain.
This does not mean you have to do nothing all day, but it does mean making conscious choices. Activities that involve prolonged sitting or little variation in posture are often stressful for the tailbone. For example, eating at home or watching a movie at home is usually more comfortable than dining out or going to the cinema, because it is easier to stand up, move around, or lie down.
Also working from home is often preferable to working in an office, as it allows you to take more frequent breaks and alternate between standing, walking, and lying down. In practice, this often means avoiding sitting as much as possible.
For practical tips and examples, you can visit the page with tips and the videos.
12. What is recommended to do when you have tailbone pain?
Anything that allows movement without provoking tailbone pain, supports the recovery.
Movement improves blood circulation, helps regulate tension in the pelvic floor, and has a positive effect on mental well-being. If a specific activity, such as walking, starts to cause pain over time, this is a sign that you have exceeded your limit. Take note of where that limit lies and, during the next activity, stay just below that duration or intensity.
Respecting these limits is an essential part of the recovery process for tailbone pain and an important element of treatment. If you would like targeted tips and advice, please visit the Tips page or make an appointment.
13. What is the best way to sit with tailbone pain?
With tailbone pain, it is often best to limit sitting as much as possible.
Pain is a signal that the load is too high, including for the tailbone, and prolonged sitting can delay recovery. Sitting slightly forward or using a tailbone cushion may reduce pressure and provide temporary relief. However, standing or lying on your side or belly, where possible, usually remains the best option.
If pain-free sitting is no longer possible, a specialised therapist can often help improve tailbone function. If you are looking for a specialised therapist, you can find one via the Appointment page.
14. Can I cycle or ride a scooter with tailbone pain?
Cycling provides movement but also places pressure on the tailbone; your body’s response is therefore decisive.
If cycling causes pain during or after the activity, it is advisable to avoid it. Certain adjustments may help such as sitting slightly further back on the saddle to reduce tailbone pressure, or leaning forward as on a racing bike. Also be mindful of bumps and potholes in the road; try to avoid them or briefly rise off the saddle.
As long as cycling does not provoke or worsen symptoms, it is generally not a problem and the movement may even support recovery. Tips on saddle position and other advice can be found on the Tips page.
15. What do I have to take into account when I want to exercise or do sports with tailbone pain?
As long as exercise does not cause additional tailbone pain during or after the activity, it is fine.
Movement contributes to flexibility and blood flow, which supports recovery. However, it is essential to listen carefully to your body’s signals. Sports that involve sitting, a risk of falling, or high tension in the gluteal muscles often provoke symptoms. Examples include rowing, canoeing, sit-ups, cycling, and heavy strength exercises such as squats and leg presses.
Other forms of movement may feel comfortable, depending on the individual. For example, breaststroke swimming may be painful while a flutter kick works well, and some yoga poses may provide relief while others increase discomfort. When in doubt, personalised advice is often helpful. You can always make an appointment at tailbonetherapist.com, including for an online consultation.
16. Should I see my general practitioner for tailbone pain?
The GP is often the first point of contact, but specialised physiotherapy usually provides clarity more quickly.
Many general practitioners and therapists have limited to no experience with tailbone pain. A specialised physiotherapist can often identify the cause more quickly and start targeted treatment immediately. Online consultations are also possible when distance is a factor. Under Appointment, you can easily find a specialised therapist.
17. Should I take pain medication for tailbone pain?
Pain medication may provide temporary relief but does not address the cause of tailbone pain.
Painkillers diminish the body’s warning signal, making it harder to sense limits, which can contribute to overloading the tailbone. Mild pain relief may sometimes help with sleep or getting through the day, but it should not be used to sit longer or be more active than the tailbone can tolerate.
Pain medication is never entirely without side effects. For medication advice, a physician is the appropriate professional. Specialised physiotherapy focuses on improving tailbone function by addressing underlying causes rather than symptom suppression, which generally leads to more sustainable results. You can read more about this approach on the page about Treatment.
18. Can tailbone pain resolve on its own?
Yes, acute tailbone pain usually resolves on its own when conditions for recovery are favourable.
When symptoms have been present for less than two months, in more than 90% of cases the body recovers spontaneously, even when a fracture is involved. A key condition is that the tailbone is sufficiently unloaded and pain is not repeatedly provoked.
If recovery stagnates and no further improvement occurs despite favourable conditions, it is advisable to consult a specialised therapist. More information can be found on the Appointment page.
19. Does tailbone pain always need treatment?
No, tailbone pain does not always require treatment; many acute complaints resolve naturally.
When tailbone symptoms have been present for less than approximately two months, the body recovers spontaneously in 90–95% of cases, even when a fracture is present. As long as you notice clear improvement and feel that recovery is underway, it is reasonable to observe the course for a while.
If recovery stagnates, symptoms remain unchanged or even worsen, consulting a specialised professional is recommended. On the Appointment page, you can easily find how to locate a specialised therapist.
20. Can anything be done about tailbone pain?
Yes, contrary to common belief, tailbone pain is often very well treatable.
There are specialised doctors and therapists who focus on treating tailbone complaints, often with good results. This does require specific knowledge and experience, which is not standard within every discipline.
More information about specialised therapists can be found on the Appointment page.
21. What treatment options are available for tailbone pain?
Tailbone pain can be treated both medically and therapeutically, each with a different approach.
Doctors often choose for medication or, in rare cases, surgery. Therapists primarily focus on improving tailbone function and mobility. Medical and therapeutic treatments can complement each other but differ fundamentally in nature.
Because knowledge about tailbone pain is limited, only a small proportion of doctors and therapists are truly specialised in treating tailbone complaints. Via the Appointment page, you can quickly find a specialised therapist.
22. Why are so few professionals specialised in tailbone pain?
Tailbone complaints are relatively uncommon and therefore receive little attention in education and research.
Most medical and paramedical training programmes devote little to no attention to tailbone pain. In addition, there is limited scientific research, partly because there is no pharmaceutical or commercial incentive. As a result, scientific confirmation of what has long been known in practice is often lacking.
At tailbonetherapist.com, treatment outcomes are carefully monitored and translated into clear, meaningful data. You can find this information on the page about Treatment.
23. Does physiotherapy help with tailbone pain?
Yes, specialised physiotherapy can be highly effective for tailbone pain.
Although scientific research is limited, extensive clinical experience shows that targeted treatment by a therapist specialised in tailbone pain can lead to significant improvement and often full recovery. At tailbonetherapist.com, treatment outcomes show that fewer than 10% of patients do not benefit and around 80% become completely pain-free.
24. What does physiotherapy for tailbone pain look like?
Physiotherapy for tailbone pain focuses on optimising the mobility and function of the tailbone.
During standard physiotherapy or even pelvic physiotherapy training, little to no attention is paid to tailbone complaints. A specialised therapist does have this knowledge and skills and examines how the tailbone moves and functions. Treatment can be done through external techniques or, in some cases, the internal (intra-anal) approach. Attention is also often given to the tension and function of the pelvic floor muscles, either through exercises or internal techniques at the pelvic physiotherapist.
At tailbonetherapist.com, only mild, external treatment methods are used. These techniques are generally painless, even when the tailbone is sensitive. More information about this approach and its results can be found on the page about the Treatment.
25. How does a medical treatment by a doctor look like for tailbone complaints?
Medical treatment primarily focuses on pain reduction and symptom control.
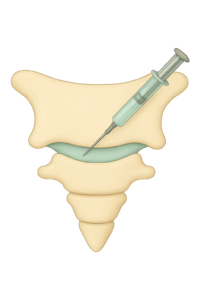
This usually involves medication, often in the form of corticosteroid injections. In some cases, a temporary or permanent nerve block may be considered. Surgical removal of the tailbone is regarded as a last resort.
On the information page about tailbone pain, more detailed information about standard medical treatment options can be found.
26. Are tailbone treatments painful?
This depends on the type of treatment used and the experience of the practitioner.
Injections can be uncomfortable or painful, but this is usually temporary. Internal treatments are often only uncomfortable when relaxation is insufficient or when the practitioner lacks experience. External manual techniques are generally mild and rarely painful, even in cases of significant tailbone sensitivity.
How uncomfortable a treatment feels is strongly related to the technique used and the skill of the therapist. At tailbonetherapist.com, treatment is provided by a highly experienced specialist.
27. What if imaging shows no abnormalities in the tailbone?
With tailbone pain, X-rays and scans often show no abnormalities.

This is because the problem usually lies in the mobility of the tailbone rather than its structure. Mobility cannot be assessed using static imaging. In addition, the tailbone is sometimes not fully or correctly visualised on imagary, or findings may be misinterpreted due to limited experience of most physicians regarding the tailbone.
A clinical examination by a specialised therapist often provides more insight than imaging alone. A specialised therapist can also help interpret imaging findings more accurately. If you would like to plan an appointment for that, this can be done through the contactform below or the page Appointment.
28. An abnormality is seen on the scan – what does that mean?
Abnormalities seen on imaging do not automatically mean they are the cause of the pain.
There is a wide natural variation in the shape, position and length of the tailbone, and no clear norm exists. Many abnormalities may have been present for years without causing symptoms. Sometimes findings are reported to provide an explanation, even though the relationship to pain is unclear or the findings are not truly abnormal, or may even be a result of the pain itself.
A specialised assessment can help clarify this and an appointment is easily made through the contactform below.
29. What can be done if the tailbone is misaligned?
An abnormal tailbone position does not necessarily cause tailbone pain.
A more forward or backward position of the tailbone can be a normal anatomical variation and is also seen in people without pain. In some cases, an apparent forward or sideways deviation is the result of pelvic floor muscle tension and resolves as pain decreases.
If pain resolves without any change in tailbone position, the position is likely not relevant to the symptoms. More information about tailbone anatomy and alignment can be found on the page about tailbone pain.
30. What can be done about tailbone deformities?
There is a wide natural variation in tailbone anatomy.
Differences in shape, length and even the number of tailbone segments are normal. The key question is always whether a visible deformity is actually related to symptoms or whether it has been present long before the pain developed. Without a clear impact as onset of the pain, deformities are rarely the cause of tailbone pain.
31. Can anything be done if the tailbone is fractured?
Even with a fractured tailbone, the body usually heals naturally.
True fractures are rare and are often confused with bruising or spraining of the tailbone joints. The most important advice is to reduce pressure on the tailbone and avoid pain to allow healing. Immobilisation, such as casting used for other fractures, is not possible for the tailbone.
If symptoms persist longer than three months, assessment by a specialised therapist is advisable. In many cases, the issue is not the fracture itself but impaired joint function, which is often treatable. At the page Appointment, you can find one easily.
32. Can tailbone pain be treated during pregnancy?
Yes, tailbone pain can be treated safely during pregnancy.
Medication, invasive treatments and even imaging are generally avoided during pregnancy. Therapeutic treatments, however, are safe due to their mild nature and can be applied effectively.
At tailbonetherapist.com, I completed additional training specifically for treating patients during pregnancy, and appointments can be made easily via the contact form below.
33. What if previous treatments have not helped?
This usually does not prevent recovery.
Many people consult here at tailbonetherapist.com after previous treatments without lasting results, yet their complaints often prove to be treatable. This is because many doctors and therapists receive little training in tailbone disorders.
Even if pelvic physiotherapy, other specialised therapists or injections have not helped, complaints are often still resolvable. There is a significant difference in experience among practitioners. In the Netherlands, the number of truly specialised tailbone therapists is small; some of them can be found in in-depth discussions on my podcasts about tailbone pain.
Through the contactform below or the page Appointment, you can make and appointment here at tailbonetherapist and are guaranteed of an experienced and specilised therapist.
34. How long does it take for tailbone pain to resolve?
Recovery time varies greatly depending on the individual and the situation.
Although patients are often told that tailbone pain simply takes a long time, acute complaints usually resolve within weeks to months. The key factor is whether the conditions for healing are present. Continued overload delays recovery, while reducing pressure allows healing to occur.
Even under optimal conditions, a small group continues to experience symptoms. In those cases, targeted treatment can often lead to recovery relatively quickly, provided a specialised therapist is involved and one of these you can easily find under Appointment.
35. What can I do myself to reduce tailbone pain?
You can help by creating optimal conditions for recovery.
This mainly involves avoiding prolonged sitting, cycling and other activities that place pressure on the tailbone or provoke pain. Using a tailbone cushion, changing positions frequently and working more while standing can help reduce symptoms.
If this is insufficient, specialised treatment is recommended and you are of course more than welkom here. Appointmens can be made through the Appointment page.
36. Should I buy a tailbone cushion?
A tailbone cushion can help reduce pressure on the tailbone while sitting.
Tailbone cushions have a cut-out at the back, and there are even chairs designed with such an opening. Ring-shaped cushions are often recommended but may actually increase pressure on the tailbone and worsen symptoms. Tailbone cushions are available in many forms and are often affordable, especially when purchased second-hand online.
An overview of different cushion types can be found in the videos on this website.
37. Which exercises help with tailbone pain?
The tailbone itself cannot be trained directly; exercises mainly focus on relaxation.
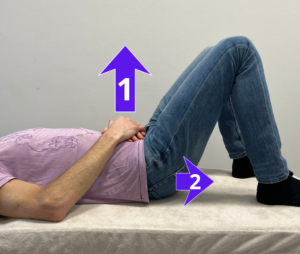
Despite claims made by a sufficient number of trainers and therapists, especially online, the tailbone itself cannot really be exercised. Tailbone pain usually relates to joint function and this cannot be actively moved in isolation. Most exercises aim to reduce tension in surrounding muscles, particularly the pelvic floor, and to create conditions that support recovery.
For tips and exercises, please refer to the page about exercises on this website.
38. Do I have a weak spot from now on once I’ve had tailbone pain?
In most cases, tailbone pain does not create a permanent weak spot.
Once the tailbone functions properly again, the body usually completes the healing process and symptoms do not return. Recurrence occurs only in a small group of people, or when treatment focuses solely on symptom relief, such as medication or pelvic floor exercises alone.
To address the underlying cause, treatment by a therapist specialised in tailbone pain is important. You can find one via the appointment page.